Hier komt de introtekst. De tekst die staat voor de “read more” waarin dus een gedeelte van het bericht al te lezen valt.
Dit is in het overzicht te lezen en is nu zo ingesteld dat na de lees meer dit intro gedeelte niet meer zichtbaar is.
<!–more–>
-
- A small transverse incision of about 5 mm is made in the full-thickness of the posterior gastric wall.
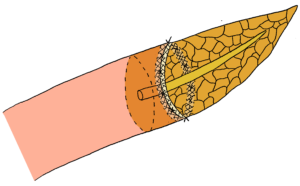
- Around the new-formed opening in the posterior wall of the stomach, a purse-string suture is placed; the distance between the purse-string suture and the incision is 1.5 times the distance between the main pancreatic duct and the edge of the pancreatic cut surface.
- A duct-to-mucosa anastomosis was performed between the main pancreatic duct and the gastric mucosa to form the inner suture-row.
- An outer suture-line was carried out by placing four sutures between the pancreatic capsule, about 2 cm away from the cut edge of the pancreas, and the seromuscular layer of the posterior gastric wall.
- The formerly placed purse-string suture is tightened gently, causing invagination of the pancreas, until the posterior stomach wall is properly wrapped around the pancreatic stump. Care is taken to avoid occlusion of the main pancreatic duct.
<ol><li><p><span style=”text-decoration: underline;”>Papillary-like main pancreatic duct invaginated pancreaticojejunostomy</span></p><ol><li><span lang=”EN-GB”>Before the anastomosis procedure is started, the pancreatic stump is prepared: the pancreatic cut surface is shaped like a ‘fish </span><span lang=”EN-GB”>mouth’ and the pancreatic duct is protruded out of the stump </span><span lang=”EN-GB”>for 6-8 mm. To do so, a 6-8 mm deep incision is performed circumferentially, 2-3 mm around the main duct, and the surrounding pancreatic parenchyma is removed. The cut end of the pancreas is closed with inverting sutures, excluding the protruded main pancreatic duct or so-called ‘papillary-like main pancreatic duct’.</span></li><li><span lang=”EN-GB”>The posterior pancreatic capsule is sutured to the seromuscular layer of the jejunum.</span></li><li><span lang=”EN-GB”>A small incision was made through the full-thickness of the jejunal wall, with a size similar to the diameter of the ‘papillary-like main pancreatic duct’.</span></li><li><span lang=”EN-GB”>Via the new-formed opening in the jejunal wall, the ‘papillary-like main pancreatic duct’ is invaginated and circumferentially fixed by 4-6 sutures, placed between the periductal parenchyma (just around the ‘papillary-like main pancreatic duct’) and the edges of the jejunal wall incision (through the full-thickness of the bowel wall). </span><span lang=”EN-GB”>Care is taken to avoid injury to the main pancreatic duct.</span></li><li><span lang=”EN-GB”>To finish the anastomosis, the anterior pancreatic capsule is sutured to the seromuscular layer of the jejunum.</span></li></ol></li></ol>
One-layered technique
DILL-RUSSELL AS. Pancreaticogastrostomy. Lancet. 1952;1:589-590
Gupta S. Pancreaticogastrostomy: A simplified technique. J Surg Oncol. 1994;56:249-250.
Using two transpancreatic sutures with buttresses
Lee JY, Kim EY, Lee JS, et al. A novel pancreaticogastrostomy method using only two transpancreatic sutures: early postoperative surgical results compared with conventional pancreaticojejunostomy. Ann Surg Treat Res. 2015;88:299-305.

