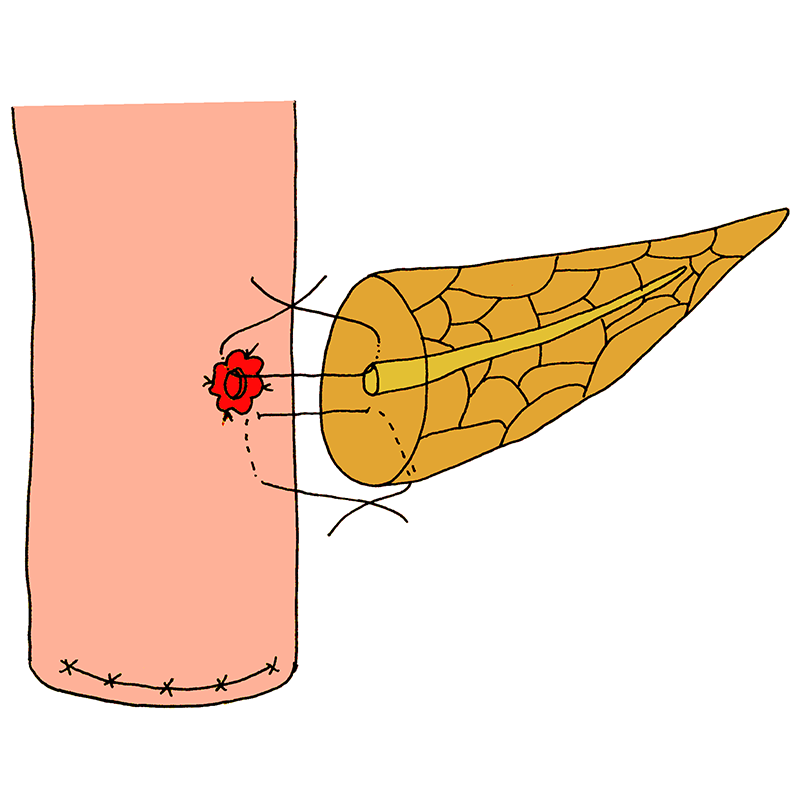
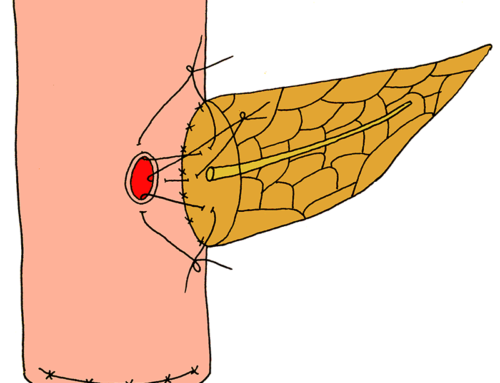
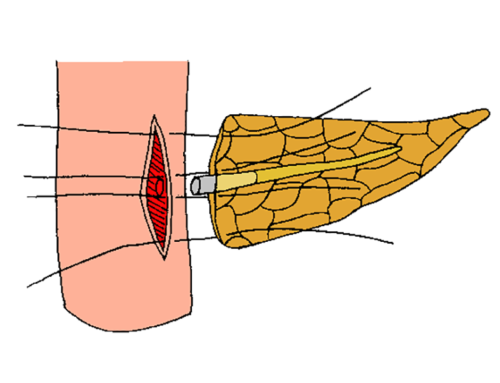
An outer, posterior suture-row is performed between the outer 2/3rd of the radius of the cut pancreatic gland and the seromuscular layer of the jejunal wall posteriorly. A small hole of 2-3 mm in diameter is made through the full-thickness of the jejunal wall, opposite the main pancreatic duct. The jejunal mucosa is everted in all directions and anchored to the seromuscular wall around the new-formed opening in the jejunum, using four stitches.
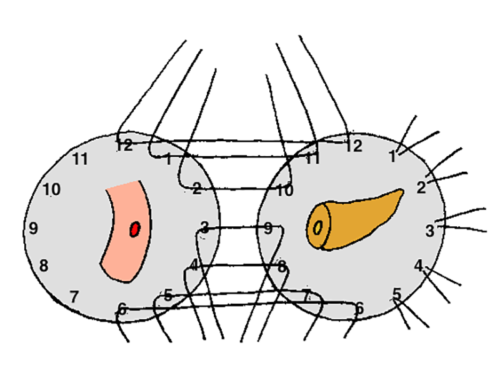
Two-layered true duct-to-mucosa pancreatojejunostomy
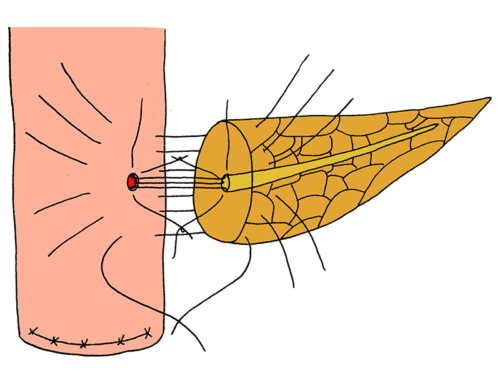
- An outer, posterior suture-row is performed between the outer 2/3rd of the radius of the cut pancreatic gland and the seromuscular layer of the jejunal wall posteriorly.
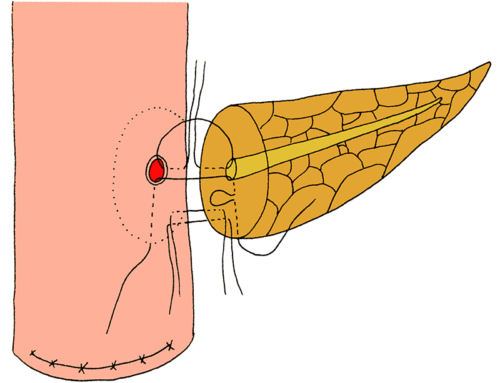
- A small hole of 2-3 mm in diameter is made through the full-thickness of the jejunal wall, opposite the main pancreatic duct.
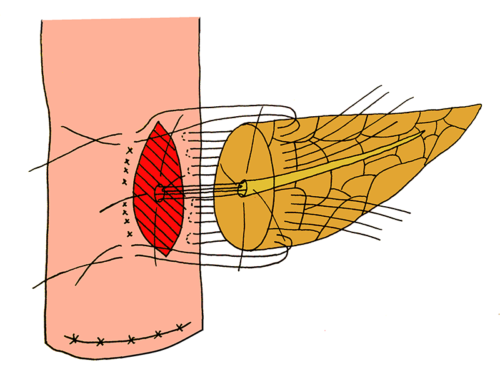
- The jejunal mucosa is everted in all directions and anchored to the seromuscular wall around the new-formed opening in the jejunum, using four stitches.
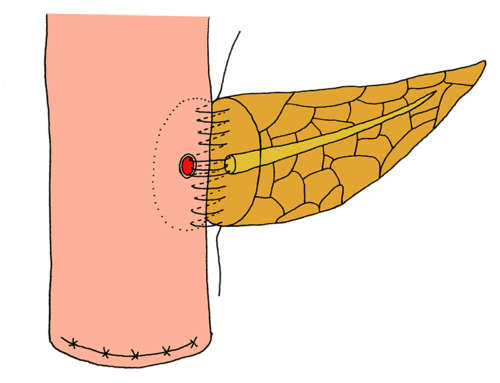
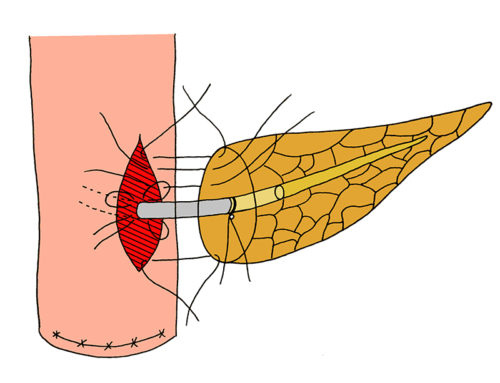
- An inner suture-row is circumferentially applied. Sutures are placed through the full-thickness of the jejunal wall, a few mm away from the jejunal opening and the everted mucosa, exciting the lumen of the jejunum via the small hole. Subsequently, the sutures penetrate the main pancreatic duct and periductal pancreatic parenchyma, including the inner 1/3rd of the radius of the cut pancreatic gland. The mucosal surfaces of the jejunum and main pancreatic duct are in close contact, featuring a ‘true duct-to-mucosa anastomosis’. Care is taken to avoid occlusion of the main pancreatic duct.
- The outer suture-row is completed anteriorly in a same fashion as with the posterior outer suture-line.
- Karavias DD, Karavias DD, Chaveles IG, Kakkos SK, Katsiakis NA, Maroulis IC. “True” duct-to-mucosa pancreaticojejunostomy, with secure eversion of the enteric mucosa, in Whipple operation. J Gastrointest Surg. 2015;19:498-505.